Published on 2025/01/06 Research powered by Mightex’s Polygon1000 

Eltanahy, A. M., Aupetit, A., Buhr, E. D., Van Gelder, R. N., & Gonzales, A. L., Light-sensitive Ca2+ signaling in the mammalian choroid. Proceedings of the National Academy of Sciences, 121(46), e2418429121 (2024).

Introduction
The choroid is a highly vascularized layer of the eye situated between the retina and sclera. It plays a crucial role in supporting retinal photoreceptors by regulating blood flow and maintaining fluid homeostasis. The absence of typical myogenic autoregulation in the choroid has led to speculation about alternative mechanisms for vascular control. This study explores whether the choroid vasculature is intrinsically sensitive to light, and proposes light-sensitive mechanisms that regulate blood flow and fluid transport, potentially affecting conditions like myopia.
Methods
The authors employed ex vivo preparations of whole choroid and eyes from transgenic mice expressing Ca2+ indicators in endothelial and mural cells. Various light wavelengths were used to stimulate tissue samples using Mightex’s Polygon DMD illuminator for spatiotemporal control of illumination, and the resulting calcium dynamics were measured. The expression of non-visual opsins (OPN3, OPN4, and OPN5) was studied using reporter mice, while violet light-induced vascular responses were examined under different intraluminal pressures.
Results
Violet light (405 nm) stimulated Ca2+ release from intracellular stores in endothelial cells of the choroid, mediated by a Gq protein-coupled receptor (GPCR) pathway involving phospholipase C (PLC) (Figure 1.). The response was abolished by inhibitors of Gq and PLC. Nitric Oxide (NO) production was also induced by violet light, and its inhibition blocked the light-induced signaling response.
Violet light also triggered Ca2+ influx in vascular smooth muscle cells (vSMCs) and pericytes, leading to arteriolar constriction. This process involved voltage-gated calcium channels (VGCCs) and was inhibited by VGCC blockers. Light and pressure interacted to regulate choroidal blood flow inversely. Increased intraluminal pressure reduced violet light-induced vasoconstriction, suggesting a novel autoregulatory mechanism where pressure counteracts light sensitivity, maintaining fluid homeostasis.
Using a double-cannulated whole-eye model, the authors demonstrated that violet light enhances trans-retinal fluid absorption into the choroid. Increased intraluminal pressure inhibited this fluid transport, but violet light exposure restored it, suggesting that light promotes ocular fluid balance.
As expected, OPN3, OPN4, and OPN5 were endogenously expressed in the choroidal vasculature. OPN3 and OPN5 were found in endothelial cells, while OPN4 was localized in mural cells. These findings suggest that non-visual opsins may play a role in the light-sensitive signaling in the choroid.
Discussion
The study introduces a dual mechanism involving light-sensitive opsins and pressure-sensitive signaling for regulating choroidal blood flow and fluid absorption. Unlike typical myogenic responses, the choroid employs an inverted autoregulatory strategy where pressure opposes light-induced vasoconstriction. This mechanism may be crucial for dark-light adaptation, optimizing oxygen delivery, and fluid clearance in the eye.
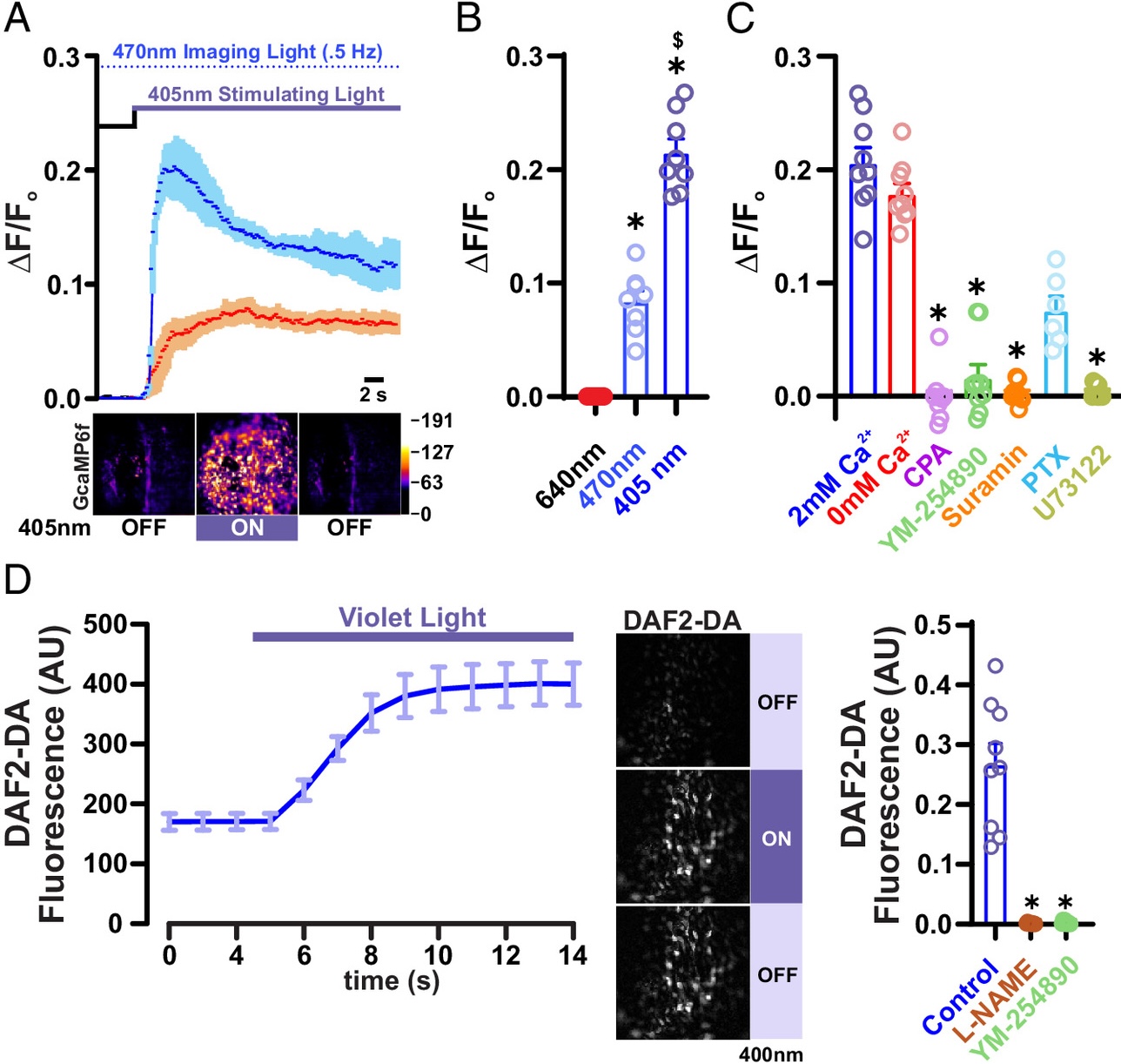
Figure 1
Francisco Rodrigues, PhD Manager, Customer Solutions at Mightex
To read the full publication, please click here.



